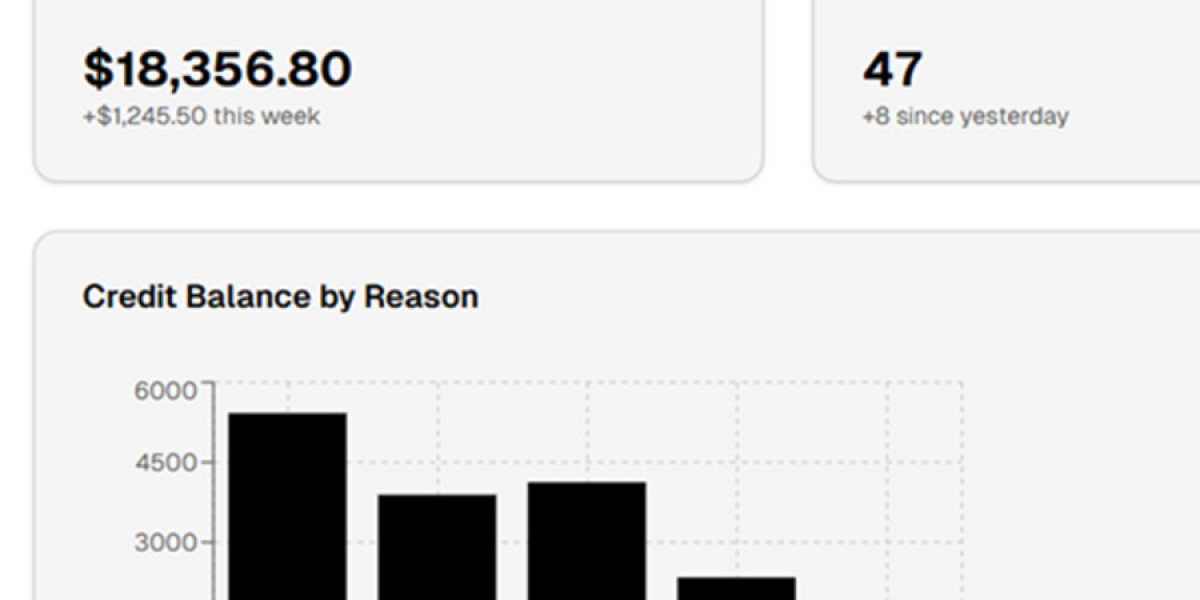
Credit balances are a common yet often overlooked challenge in healthcare revenue cycle management. A credit balance occurs when payments received exceed the charges billed, resulting in overpayments from insurance companies or patients. If not properly managed, these credits can lead to compliance risks, financial inaccuracies, and revenue leakage.
One of the main causes of credit balances includes duplicate payments, incorrect contractual adjustments, coordination of benefits errors, and posting mistakes. While some credits are valid and require refunds, others may indicate deeper issues within the billing or payment posting process.
Effective credit balance management ensures that overpayments are identified, validated, and refunded promptly. Regulatory bodies and payers closely monitor how providers handle credit balances, making compliance a critical factor. Failure to issue timely refunds can result in penalties, audits, and reputational damage.
Outsourcing credit balance services allows healthcare providers to focus on patient care while experienced RCM professionals handle complex credit analysis. A dedicated credit balance team performs detailed research, communicates with payers, and ensures proper documentation for every refund issued.
Another key advantage of professional credit balance services is root cause analysis. By identifying patterns behind recurring credits, providers can correct workflow gaps and prevent future revenue loss. This leads to cleaner accounts, improved reporting accuracy, and stronger financial performance.
In today’s complex healthcare billing environment, credit balance resolution is not optional—it is essential. Partnering with a reliable credit balance service provider helps healthcare organizations maintain compliance, protect revenue, and optimize their revenue cycle.