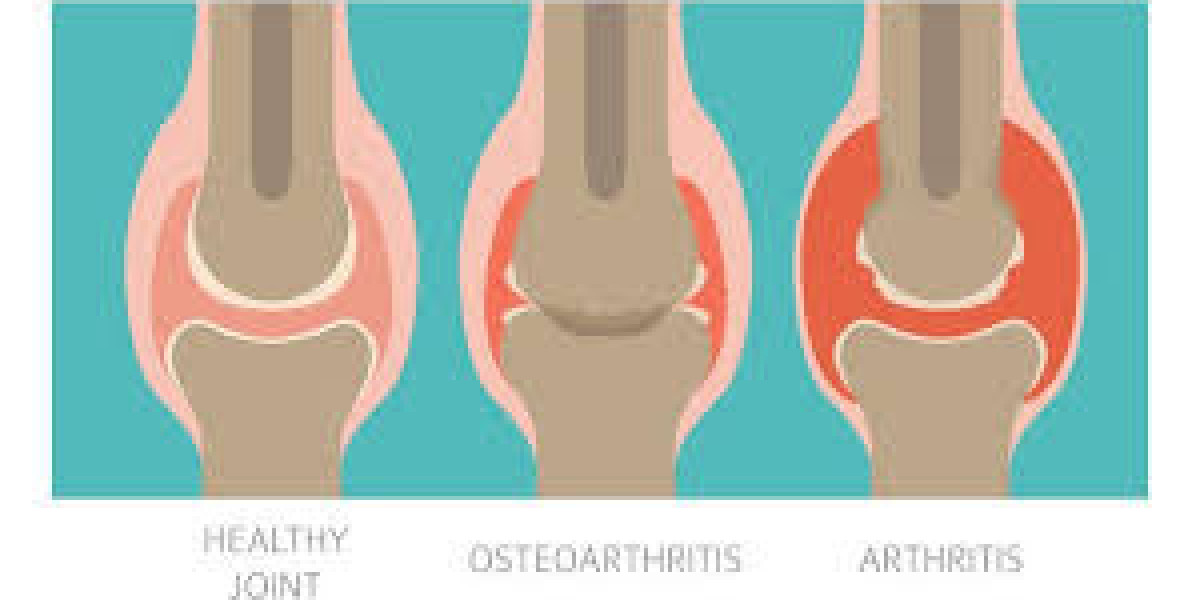
Osteoarthritis (OA) is the most common form of arthritis, affecting over 32 million adults in the United States and millions more worldwide. Often called “wear-and-tear” arthritis, OA occurs when the protective cartilage that cushions the ends of your bones gradually breaks down.
Carticlas tablets are a cutting-edge dietary supplement formulated to promote joint health, reduce inflammation, and support overall well-being. They are designed to address the common issues associated with aging, high physical activity, and other factors that affect joint and bone health.
While OA cannot be cured, understanding the condition and taking proactive steps can help you manage pain, maintain mobility, and enjoy a better quality of life.
What Is Osteoarthritis?
Unlike inflammatory arthritis (such as rheumatoid arthritis), OA is characterized by the degeneration of joint cartilage and underlying bone. Over time, this process leads to:
Joint pain during or after movement
Stiffness, particularly upon waking or after periods of inactivity
Loss of flexibility, making daily tasks challenging
Grating sensations or bone spurs that develop around the affected joint
Although it can affect any joint, OA most commonly targets the knees, hips, hands, and spine.
Who Is at Risk?
Several factors increase your likelihood of developing OA:
Age: Risk rises after age 45.
Genetics: Family history can predispose you to weaker cartilage.
Joint injury or overuse: Sports injuries or repetitive jobs strain joints.
Obesity: Excess weight places added stress on weight-bearing joints.
Gender: Women are more prone to OA, especially after menopause.
Recognizing your personal risk can prompt earlier interventions and lifestyle adjustments.
Diagnosis and Monitoring
OA is usually diagnosed based on:
Medical history and a review of symptoms (pain patterns, stiffness).
Physical examination, assessing joint flexibility, swelling, and alignment.
Imaging tests like X‑rays or MRI, which reveal cartilage loss, bone spurs, and joint space narrowing.
Lab tests to rule out other types of arthritis.
Regular follow‑ups with your healthcare provider will help monitor disease progression and adjust your management plan as needed.
Management Strategies
Although there’s no cure for OA, a combination of treatments can relieve symptoms and improve function:
1. Lifestyle and Self‑Care
Weight management: Losing even 5–10% of body weight can significantly reduce joint stress.
Low‑impact exercise: Swimming, cycling, and walking strengthen muscles and improve flexibility without overloading joints.
Hot/cold therapy: Warm baths and heating pads ease stiffness, while cold packs reduce swelling.
2. Physical and Occupational Therapy
Targeted exercises build muscle support around the joint.
Assistive devices (braces, shoe inserts, canes) protect and stabilize affected areas.
Ergonomic adjustments in the workplace or home minimize joint strain.
3. Medications and Supplements
Over‑the‑counter pain relievers: Acetaminophen or NSAIDs (ibuprofen, naproxen) control mild to moderate pain.
Topical agents: Creams containing capsaicin or NSAIDs deliver relief directly to the joint.
Supplements: Glucosamine and chondroitin may benefit some patients, though research is mixed. Always consult your doctor before starting any supplement.
4. Procedures and Surgery
Joint injections: Corticosteroids or hyaluronic acid can temporarily reduce inflammation and improve lubrication.
Surgical options: In advanced cases, arthroscopy to smooth joint surfaces or joint replacement (knee, hip) can restore function and relieve pain.
Coping Tips and Support
Living with OA extends beyond medical treatments—you’ll also benefit from:
Stress management: Techniques like meditation, deep breathing, and counseling address the emotional toll of chronic pain.
Support networks: Joining arthritis support groups or online communities connects you with others facing similar challenges.
Education: Staying informed about new therapies, exercise programs, and assistive technologies empowers you to advocate for your health.
Final Thoughts
Osteoarthritis may be a lifelong condition, but it doesn’t have to define your life. By understanding the disease process, identifying risk factors, and embracing a multifaceted management plan, you can minimize pain, maintain joint function, and continue doing the activities you love. Work closely with your healthcare team, stay proactive in self-care, and remember—small, consistent steps often yield the most meaningful improvements.